TOP MYTHS & FACTS ABOUT FOOD AND DIABETES
Food and Diabetes: Top Myths and Facts Many myths surround diabetes, especially when it comes to food and diabetes. This makes it hard to figure out what you can and cannot eat. Are carbs bad for you? Are you allowed to eat sweets? Do you have to follow a special diet? To make things easier, here’s a look at the facts behind some of the top myths surrounding food and diabetes. Myth #1 – Eating Sugar Can Cause Diabetes...
Read MoreDiabetes Basics
Understanding the basics of diabetes is the first step in gaining control of your health. Let’s look at what causes diabetes, some of the common symptoms, the benefits of healthy living, and what to do if you’ve just been diagnosed. What is diabetes? Diabetes is a medical condition in which the blood glucose levels remain persistently higher than normal. It is becoming more common in Singapore. This may be due in part to ageing population, unhealthy diets and lack of exercise. Insulin is a hormone produced by the pancreas that allows your body cells to use blood glucose for energy. Food is converted...
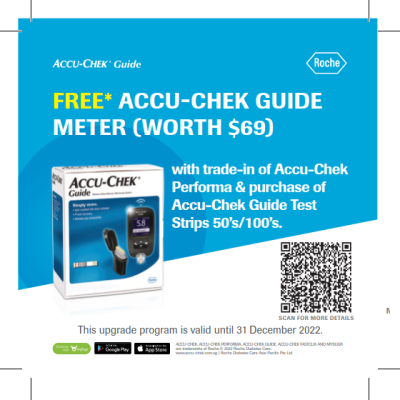
Read MoreSelf-monitoring of your diabetes
Diabetes is part of your everyday life. Appropriate self-monitoring can help you manage your daily blood glucose, and better adapt your lifestyle and treatment to suit your needs.1 The more often you check your blood glucose, the better you will understand it and the easier it will be for you to manage your diabetes. It doesn’t matter if you have type 1 or type 2 diabetes, or if you are taking insulin or not, self-monitoring can help you and your doctor manage your therapy.2 By managing your diabetes, you reduce the risk of developing complications. That means potentially less eye, kidney and...
Read MorePatient Experience Sharing
Accu-Chek integrated diabetes management solution meaningfully supports people with diabetes in their diabetes management journey in Singapore. Hope their personal journey sharing inspires and motivates you and your loved ones! ...
Read MoreHow to make sense of blood sugar numbers
I don’t understand what my blood sugar range means! If you live with diabetes, you have probably been asked to check your blood sugar a lot. But what are you supposed to be checking? How do you make sense of the numbers you see? Managing your diabetes is easier when you know what the numbers mean and what you are trying to accomplish....
Read MoreDiabetics Stay healthy during COVID-19
Learn more about the safety measures against COVID-19 for people living with diabetes.
Read More5 DIABETES-FRIENDLY BREAKFAST FOOD
If you have diabetes, it’s time to overhaul your morning meal. Why? Studies show eating breakfast lowers your chance of overeating throughout the day.1 Of course, you’ve got to pick the right foods. Many popular breakfast foods have sugars and carbs — which can spike your blood sugar. You’ll also want to avoid...
Read MoreSay 'No' to Foot Complaints
Managing diabetes can be complex, but it shouldn’t mean missing out on the good things in life, like feeling the scrunchy sand under your feet, dipping your feet surf, long hikes in the park with your family. Keeping blood glucose levels within range can help prevent complications such as those that affect your feet1. High blood glucose can cause nerve damage (neuropathy) especially in the limbs (example both legs and feet). In addition, poor circulation caused by diabetes may lead to more serious problems like diabetic foot ulcer and infections and even deformity of the feet...
Read MorePages
Diabetes Basics
Understanding the basics of diabetes is the first step in gaining control of your health. Let’s look at what causes diabetes, some of the common symptoms, the benefits of healthy living, and what to do if you’ve just been diagnosed. What is diabetes? Diabetes is a medical condition in which the blood glucose levels remain persistently higher than normal. It is becoming more common in Singapore. This may be due in part to ageing population, unhealthy diets and lack of exercise. Insulin is a hormone produced by the pancreas that allows your body cells to use blood glucose for energy. Food is converted...
Read MoreSelf-monitoring of your diabetes
Diabetes is part of your everyday life. Appropriate self-monitoring can help you manage your daily blood glucose, and better adapt your lifestyle and treatment to suit your needs.1 The more often you check your blood glucose, the better you will understand it and the easier it will be for you to manage your diabetes. It doesn’t matter if you have type 1 or type 2 diabetes, or if you are taking insulin or not, self-monitoring can help you and your doctor manage your therapy.2 By managing your diabetes, you reduce the risk of developing complications. That means potentially less eye, kidney and...
Read MorePatient Experience Sharing
Accu-Chek integrated diabetes management solution meaningfully supports people with diabetes in their diabetes management journey in Singapore. Hope their personal journey sharing inspires and motivates you and your loved ones! ...
Read MoreHow to make sense of blood sugar numbers
I don’t understand what my blood sugar range means! If you live with diabetes, you have probably been asked to check your blood sugar a lot. But what are you supposed to be checking? How do you make sense of the numbers you see? Managing your diabetes is easier when you know what the numbers mean and what you are trying to accomplish....
Read MoreDiabetics Stay healthy during COVID-19
Learn more about the safety measures against COVID-19 for people living with diabetes.
Read More5 DIABETES-FRIENDLY BREAKFAST FOOD
If you have diabetes, it’s time to overhaul your morning meal. Why? Studies show eating breakfast lowers your chance of overeating throughout the day.1 Of course, you’ve got to pick the right foods. Many popular breakfast foods have sugars and carbs — which can spike your blood sugar. You’ll also want to avoid...
Read MoreSay 'No' to Foot Complaints
Managing diabetes can be complex, but it shouldn’t mean missing out on the good things in life, like feeling the scrunchy sand under your feet, dipping your feet surf, long hikes in the park with your family. Keeping blood glucose levels within range can help prevent complications such as those that affect your feet1. High blood glucose can cause nerve damage (neuropathy) especially in the limbs (example both legs and feet). In addition, poor circulation caused by diabetes may lead to more serious problems like diabetic foot ulcer and infections and even deformity of the feet...
Read More